Trends in Specialty Drug Benefit Design: Rebates
Posted on June 6, 2022
Employers are navigating a fast-changing landscape of specialty drug benefits. Specialty drug patients now make up 4% of commercially insured member populations as of 2020, up from 3.7% in 2018, and specialty drug spend has now reached 50% of total drug spend. Employers are trying to achieve the right balance of supporting their employees with necessary medications, while managing costs and maintaining affordability of benefits.
A new report from the Pharmaceutical Strategies Group (PSG), “Trends in Specialty Drug Benefit Design Report,” shares the latest findings and insights from a survey of 171 benefits leaders of plan sponsors. These plan sponsors represent approximately 41.4 million covered lives. This research shows the latest thinking of industry leaders as they evaluate their options to support people while managing the rising costs of specialty drugs.
Let’s take a closer look at specialty drug rebates and what they mean for specialty drug benefit design.
Specialty drug rebates: still a common method to control costs
Rebates continue to be an important aspect of managing the costs of specialty drugs. These rebates usually get negotiated as part of the overall formulary contracting agreement with the Pharmacy Benefit Manager (PBM) or health plan. PBMs will sometimes pass on a portion of the savings – or all of the savings – to the plan sponsor, depending on the contract. This is one-way rebates can help reduce the plan sponsor’s net specialty prescription drug costs as part of their pharmacy and medical benefits. Manufacturers determine these rebates or other negotiated price concessions based on formulary placement, predicted volume of specialty drugs, and other considerations.
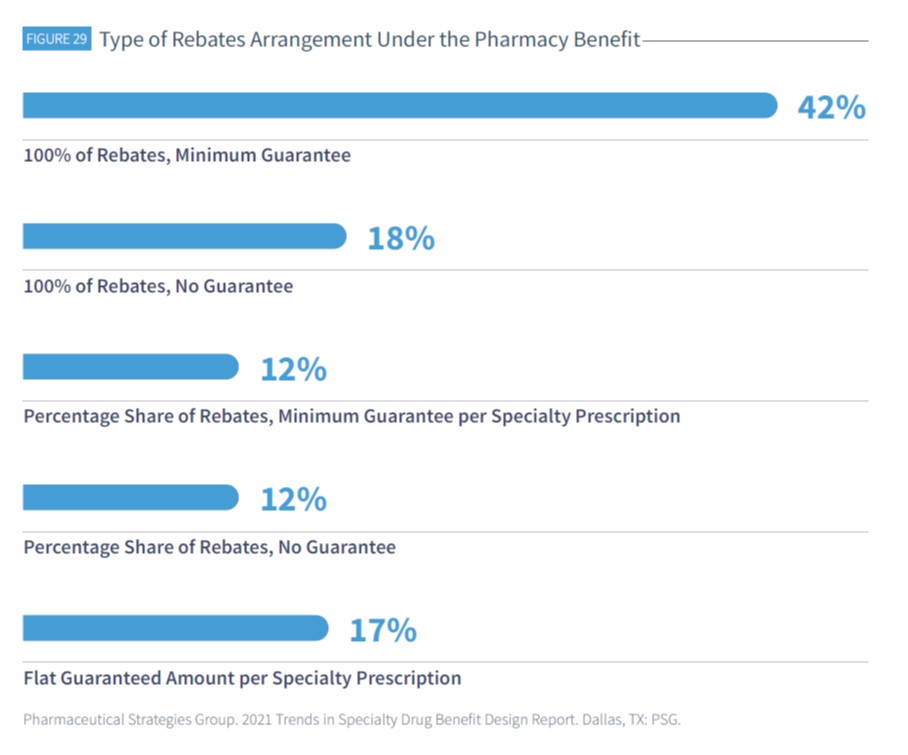
The terms of the specialty drug rebate will also depend on the client contracts. PBM contracts might specify a guaranteed flat dollar amount or percentage share of rebates (which might or might not include minimum guarantees), “per prescription,” or “per rebateable drug.”
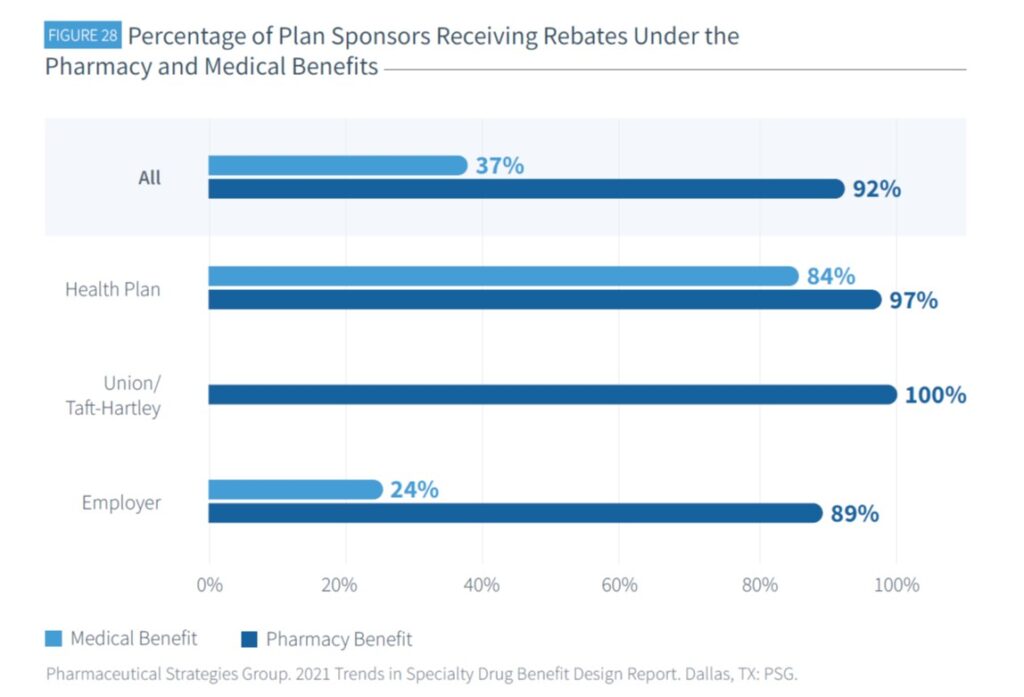
Pharmacy benefit specialty drug rebates are being received by 92% of plans
Among plan sponsors with specialty drug coverage in the pharmacy benefit, 92% receive rebates, compared to 37% receiving rebates under the medical benefit. Health plans are more likely to receive rebates under the medical benefit than employers or union/Taft-Hartley plans.
Under the pharmacy benefit, 60% of plans receive 100% of rebates
Among plan sponsors who reported receiving rebates for specialty drugs under the pharmacy benefit and who are also aware of the rebate arrangement, 42% reported receiving 100% of rebates with a minimum guarantee.
47% of plans’ rebate guarantees felt the effect of not using their PBM’s specialty pharmacy
Plans are typically expected to use their PBM’s specialty pharmacy on an exclusive basis in order to maximize their rebates. The PSG survey found among plans with a flat or minimum per specialty prescription guarantee, 47% said using other specialty pharmacies outside of their PBM affected their rebate guarantees.

Beyond rebates: strong interest in alternatives
Although rebates are still a common approach to managing specialty drug costs, the survey found they are not the only possible solution. PSG’s report investigated the level of interest in alternatives to rebates for specialty drugs.
The survey found significant demand for rebate alternatives. 57% of respondents said they were “very interested” in requiring 100% pass-through of rebates and discounts to plan sponsors. 49% said they were “very interested” in eliminating rebates and replacing them with upfront discounts. However, there was less interest in requiring patients to share rebates at point-of-sale; only 17% of respondents said they were “very interested” in this option.
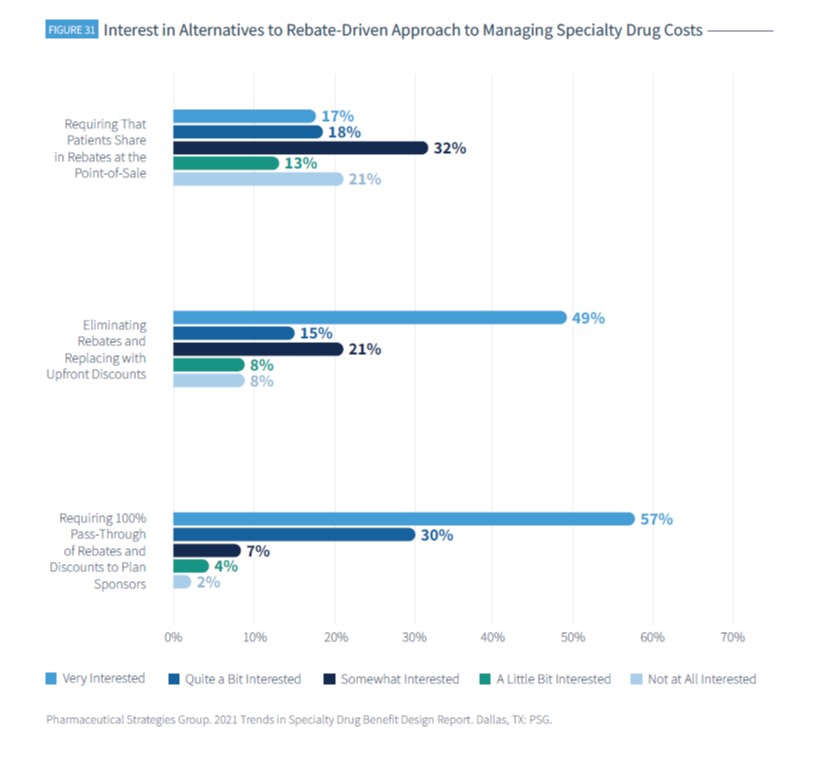

However, if you look at the survey results in aggregate, there is strong demand to ensure rebates are optimized within specialty drug benefit landscape. 87% of respondents were “very interested or quite a bit interested” in requiring 100% pass-through of rebates and discounts to plan sponsors, and 64% shared this same level of interest in eliminating rebates and replacing them with upfront discounts.
Rebates may still have a place, for now, in the world of specialty drug benefit design. But there is a clear appetite for change. Plan sponsors and PBMs have an opportunity to rethink the model for managing these costs while continuing to support access to specialty prescription drugs for the patients who need them.
Download the Trends in Specialty Drug Benefit Design Report to learn more about the high interest in alternatives to the rebate-driven approach to managing specialty drug costs.
Download 2023 Trends in Specialty Drug Benefits Report
"*" indicates required fields

