Highlights from the 2019 PBMI Trends in Specialty Drug Benefits Report: Why Specialty Drug Cost-Sharing Is a Balancing Act for Plan Sponsors
Posted on April 23, 2019
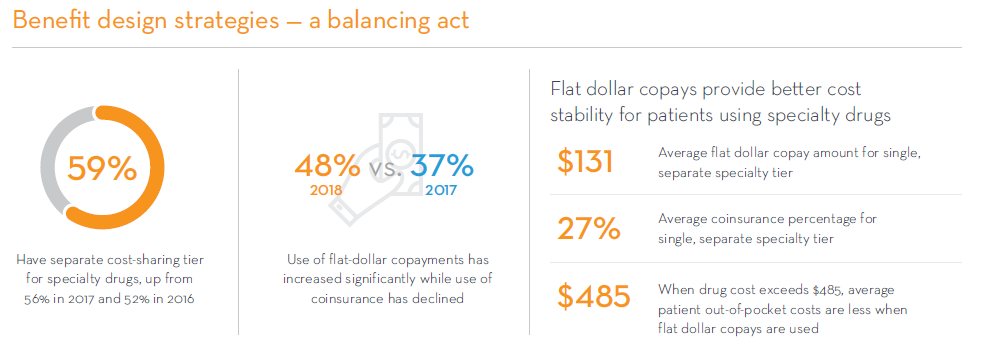
For the past eight years, PSG’s Pharmacy Benefit Management Institute (PBMI) has produced original research focused on specialty drug benefit designs used by employers, unions, and commercial health plans across the country. As mentioned in an earlier blog post, the percentage of members using specialty medications has grown in the last few years, yet they still only represent 4.9% of member populations.1 Less than 5% of members represent 50% of ALL drug costs,2 creating challenges for plan sponsors who must balance access and affordability for members who use specialty drugs with premiums and other-cost-sharing for all members. How are they doing this? One way is through the use of cost-sharing aimed at specialty drugs. In 2018, 59% of plan sponsors reported having a separate cost-sharing tier for specialty drugs, up from 52% in 2016.
However, plan sponsors recognize the burden of high drug costs on their members. In 2018, the use of flat-dollar copayments increased significantly while the use of coinsurance declined. The average flat dollar copay amount for a single, specialty tier was $131 in 2018. This can be compared to the average coinsurance percentage for a single, specialty tier of 27%. When the cost of the drug exceeds $485, out of pocket costs for the member is less when a flat-dollar copayment is used. Considering that the average price of a specialty drug claim in 2017 was $4,774, 3 the out-of-pocket costs for a member with coinsurance would be $1,289 for a single prescription. Research clearly shows the correlation between high out-of-pocket costs and abandonment rates for medications, even in life-threatening conditions such as cancer.4
About 1 in 4 adults taking prescription medications in the U.S. report having a difficult time affording their medication.5 The percentage of those using specialty drugs having difficulty with affordability is significantly higher. Copay assistance programs are one solution that many consumers have turned to, with 67% of plan sponsors reporting that their members use copay cards offered by pharmaceutical manufacturers. Copay assistance programs, however, can come with their own set of challenges for plan sponsors, as we will discuss in our next blog post in this series highlighting key trends from PBMI’s 2019 Specialty Drug Benefits Report.
For more details on other trends in specialty drug management, download your free copy of the report at www.pbmi.com/specialtyreports.
Read the previous article in this series:
[1] Pharmaceutical Strategies Group. Artemetrx State of Specialty Spend and Trend, 2017 Results. September 2018. https://www.psgconsults.com/specialtyreport/?gclid=EAIaIQobChMIpqyWoZHl3QIVkAFpCh19eQBrEAAYASAAEgIrlfD_BwE.
[2] Prime Therapeutics. The Inevitable Increase in Specialty Growth. November 14, 2017. https://www.primetherapeutics.com/en/news/prime-insights/2017-insights/insights-specialty-infographic.html.
[3] Pharmaceutical Strategies Group. Artemetrx State of Specialty Spend and Trend, 2017 Results. September 2018. https://www.psgconsults.com/specialtyreport/?gclid=EAIaIQobChMIpqyWoZHl3QIVkAFpCh19eQBrEAAYASAAEgIrlfD_BwE.
[4] Doshl JA, Li P, Huo H, et al. Association of patient out-of-pocket costs with prescription abandonment and delay in fills of novel oral anticancer agents. Journal of Clinical Oncology. 2018; 36(5):476-482.
[5] Peterson-Kaiser Health System Tracker. What are the recent and forecasted trends in prescription drug spending? https://www.healthsystemtracker.org/chart-collection/recent-forecasted-trends-prescription-drug-spending/#item-start. Data from KFF Health Tracking Poll (conducted Feb 14-24, 2019). Accessed April 16, 2019.

