Spotlight on Utilization Management with Sharon Phares, PhD, MPH & Stephen Mackie
Posted on December 1, 2021
Utilization management (UM) programs are a vital tool in the clinical and cost management of drugs. These programs are offered in various forms by most pharmacy benefit managers (PBMs). Typically, there is an additional charge, but the value proposition purports these programs save overall costs by ensuring appropriate utilization. Because of their importance, this year’s report takes a closer look at satisfaction with UM programs.
Three themes emerged when respondents shared what PBMs could do to improve satisfaction with UM programs:
- Lower or no cost for programs
- Better reporting
- More thoughtfully approaching improvement of member experience
Current Landscape of UM
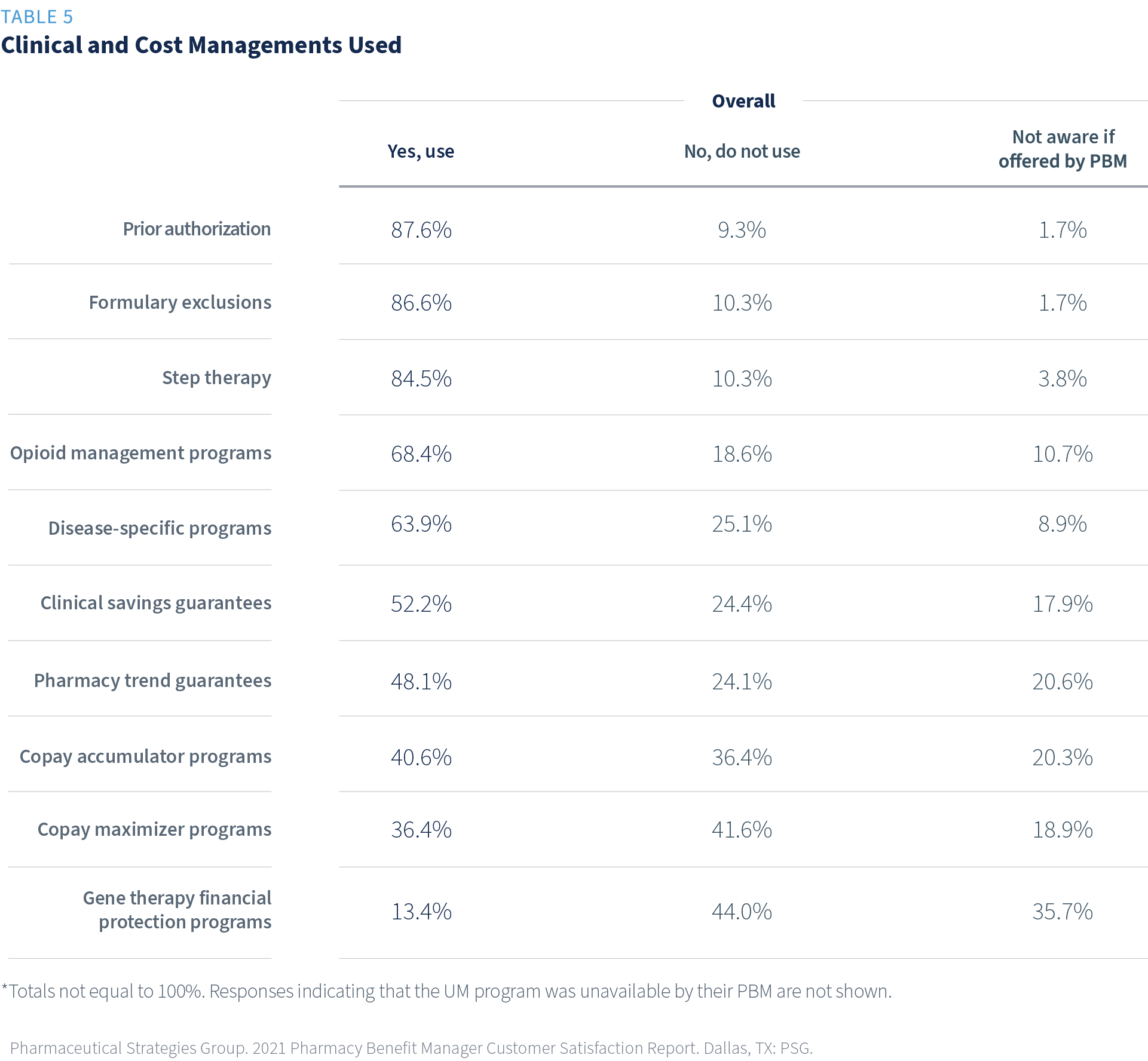
More than two-thirds of respondents reported they currently use prior authorization (PA) (88%), formulary exclusions (87%), step therapy (85%), and opioid management programs (69%).
The least frequently used program is gene therapy financial protection programs (13%). It also has the least awareness (36% not aware if offered by PBM).
No significant differences by size of PBM were found.
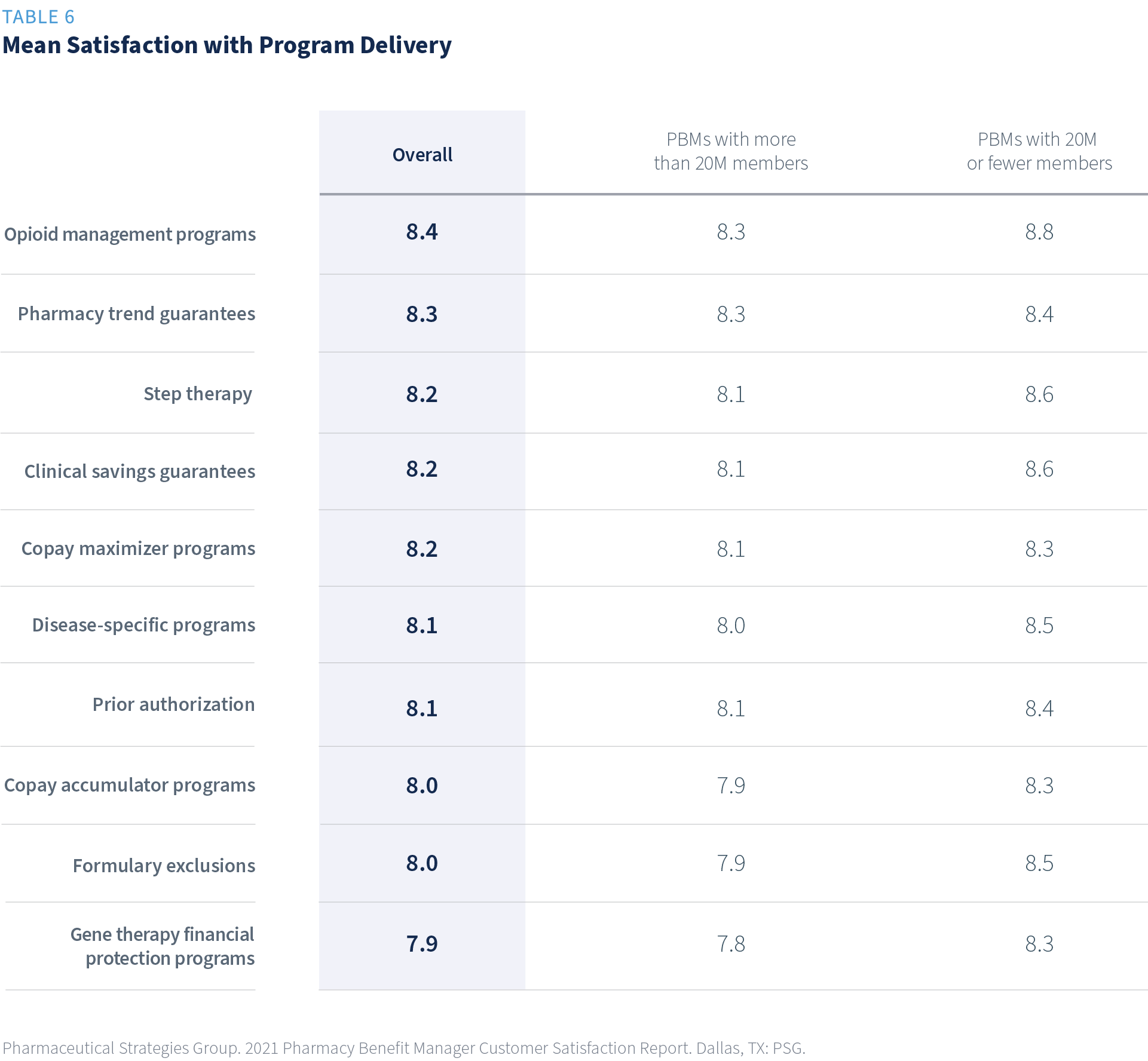
Satisfaction with UM Program Delivery
The satisfaction with promised savings is highest for opioid management programs, clinical savings guarantees, pharmacy trend guarantees, and gene therapy financial protection programs.
Satisfaction with UM Program Savings and Member Experience
Average satisfaction with member experience for programs with little to no member impact, such as savings guarantees, were rated highest. On the other hand, programs with a more direct member impact, such as step therapy and copay accumulator programs, ranked lower in satisfaction.


Satisfaction with UM Program Reporting
Receiving timely, understandable, and accurate reporting provides plan sponsors with the information they need to know if a program is working as expected. Appropriate reporting provides evidence of value. Respondents whose organizations are currently using a program revealed their satisfaction was highest with gene therapy financial protection programs (8.3), followed by pharmacy trend guarantee (8.2). Step therapy reporting ranked lowest at 7.6.

Forward-looking Recommendations
Let’s return to the three key takeaways that emerged from this research about how PBMs could improve satisfaction with UM programs (lower or no cost for programs; better reporting; and more thoughtfully approaching improvement of member experience).
This respondent quote illustrates plan sponsor insights around improving member experience:
Cost management programs always seem to penalize the member and make things harder on them. For example, PA is required for an adult on Adderall. I have never seen it not approved; it just makes the member and the physician jump through hoops. And our plan is not getting any big impact from this requirement.
UM satisfaction is highest for the UM programs that provide cost-savings for plan sponsors without significantly impacting their members at the pharmacy counter or interrupting therapy. Plan sponsors need to balance the cost savings and member experience. It is a tricky balancing act.
Download the 2021 PBM Customer Satisfaction Report
Review the complete report to learn more about how your plan can strike the right balance.

Download the 2021 PBM Customer Satisfaction Report
About the 2021 PBM Customer Satisfaction Report
This annual report summarizes overall satisfaction with pharmacy benefit managers (PBM) and satisfaction with over 40 PBM functions and services beyond overall satisfaction. It is the most comprehensive research of its type for the PBM space. This report is widely recognized for the comparative information it provides to benefit executives responsible for researching, selecting, and managing PBMs.

