Breaking News: New Weight Loss Drug, Wegovy™ (Semaglutide), Approved by FDA
Posted on June 24, 2021
What payers and plan sponsors need to know about the “most effective drug” for weight loss
What is happening?
Novo Nordisk announced the U.S. Food and Drug Administration (FDA) approval of Wegovy™ (semaglutide) for obesity on June 4, 2021.
- Wegovy is indicated as an adjunct to a reduced-calorie diet and increased physical activity for chronic weight management in adults with a:
- Body mass index (BMI) of ≥30 kg/m2, which is considered obese; or
- BMI ≥27 kg/m2, which is considered overweight, in the presence of weight-related comorbidity (i.e., hypertension, type 2 diabetes, high cholesterol)
- Wegovy is the newest version of semaglutide, which has been available as Ozempic® and Rybelsus® for the treatment of type 2 diabetes
- Wegovy is administered as a once-weekly subcutaneous injection and is available as a pre-filled single-dose pen
- A maintenance dose is 2.4mg weekly
Why is this important?
- Wegovy is being touted as the “most effective drug” for weight loss and estimated it could help patients lose 15 percent of excess body weight in one year
- Studies have shown weight loss of 5 percent or more has had an impact on weight-related comorbidities
- In Wegovy clinical trials, 83.5 percent of patients achieved 5 percent or more bodyweight reduction with an average weight loss of 14.9 percent of body weight at 68 weeks
- Wegovy is estimated to cost $1300/month, $15,600 per patient per year
- An estimated 100 million adults in the U.S. live with obesity, and one in three adults struggle with obesity
- Many plan sponsors have traditionally considered weight-loss drugs to be lifestyle drugs and excluded them from coverage
- Obesity is regarded as a gateway disease associated with at least 60 other serious health conditions and decreased life expectancy
- Obesity is now considered a chronic disease and has been designated a chronic disease by the following organizations:
- American Medical Association (AMA)
- American Academy of Family Physicians (AAFP)
- American Association of Clinical Endocrinology (AACE)
- The Obesity Society (TOS)
- Word Obesity Federation (WOF)
Key Takeaways and Next Steps
The coverage of weight-loss drugs is now under consideration by some plans due to the positive outcomes Wegovy has achieved in clinical trials. Plans hope weight loss will result in improved health outcomes.
The decision to cover (or not cover) weight-loss drugs belongs with each payer or plan sponsor based on what is best for their patient population.
For those who choose to cover Wegovy, PSG recommends the following:
- Thoroughly evaluate the financial impact of covering weight loss drugs
- Better outcomes are expected when Wegovy is combined with other weight management strategies. PSG suggests the inclusion of those strategies within prior authorization (PA) criteria. (See more PA best practices below.)
- Limit supply to 30-days per claim, as the drug can be difficult to tolerate, especially at first
- Implement stringent PA criteria and include the collection of documentation where applicable to confirm criteria. Best PA practices for Wegovy include:
- Diagnose obesity and include current BMI
- Document baseline weight as required by renewal criteria
- Specify Wegovy will be used in combination with a reduced-calorie diet and exercise program for optimal results
- Allow short initial approval duration (three months maximum)
- The clinical trials used a 68-week period, collecting and reporting data up to 68 weeks
- However, the drug is indicated for “chronic” weight management in adults, which opens the door to an indefinite duration of use
- There were reports of weight gain following discontinuation of Wegovy after the clinical trial ended
- Require percentage weight loss reduction for continued approval
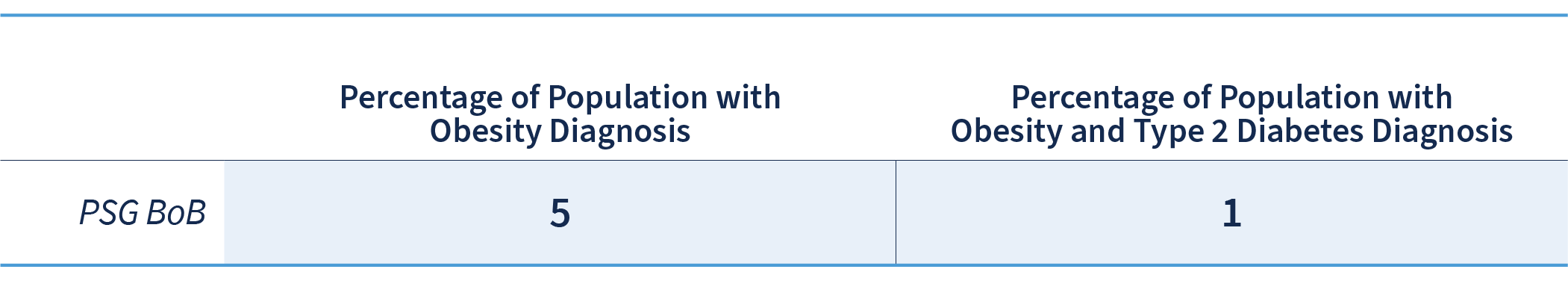
The scope of utilization could feel daunting to plan sponsors with one in three Americans currently struggling with obesity. PSG’s analytics team identified the number of members diagnosed with obesity and the representation (percentage) of the overall membership (for integrated clients).
- Across the PSG Book of Business, 5 percent of members have a diagnosis of obesity
- The members diagnosed with obesity and type 2 diabetes are also identified because they may already be on a GLP-1 receptor agonist, making them ineligible candidates for Wegovy
- These numbers do not consider members who maybe be overweight and have at least one weight-related comorbid condition, who may be candidates for Wegovy.
Connect with your PSG clinical consultant to proactively manage Wegovy and make the best decisions for your unique plan.
Not a current PSG client? Engage our clinical team to:
- Assess the potential impact of Wegovy on your population
- Make an informed decision about coverage
- Plan how to manage the drug for optimal financial and clinical outcomes

