Highlights from PBMI’s 2018 Trends in Specialty Drug Benefits Report
Posted on March 6, 2018
Understanding Why Cost Concerns Continue
For the last 7 years, PSG’s Pharmacy Benefit Management Institute (PBMI) has produced original research focused on specialty drug benefit designs used by employers across the country. As the primary payer of health and drug benefits for non-elderly Americans,[1] employers must juggle their desire to provide valuable drug benefits to employees, retirees, and family members while managing costs. This is more difficult than ever in a marketplace where specialty drug prices continue to soar with no end in sight. Thus, it is not surprising that 61% of employers report that managing specialty drug costs is their number one priority when it comes to specialty drug benefits.
61% of respondents list management of
specialty drugs as their number one priority
Some might think that focusing on cost management first is not the right way – aren’t we supposed to think about improving clinical outcomes first? People before hard dollars? Consider a few rather startling statistics and the need to focus on cost management becomes clear:
- Specialty drugs are expected to account for half of total U.S. drug spend by 2020 even though only 1% to 2% of Americans use specialty drugs
- Specialty drug costs have increased 55% under the medical benefit since 2011 and double-digit annual specialty trend under the pharmacy benefit is the norm, not the exception
- In the next 15 years, the cost to employers of providing healthcare benefits are expected to exceed wages
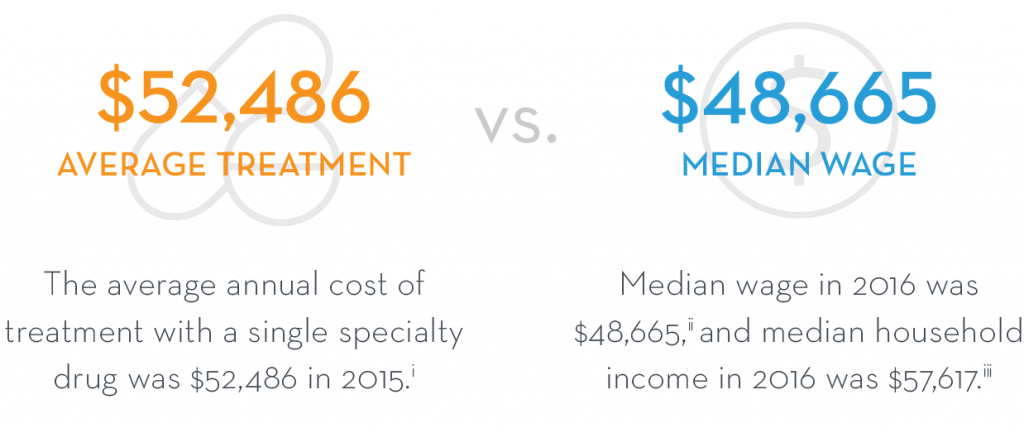
- And for members using specialty drugs, the average annual cost of a single specialty drug already exceeds wages
Employer concerns about specialty drug affordability are escalated when considering orphan drugs. Orphan drugs are those used to prevent, diagnose, or treat a disease or condition that affects fewer than 200,000 Americans. Orphan drugs can be life-extending or life-saving for patients suffering from conditions that previously had no treatment, but they also come with a steep price. The average annual cost of an orphan drug per patient was $140,000 in 2016.[2] Individual drugs can be much higher. For example, Soliris®, which treats a rare blood disorder, costs up to $400,000 annually but helps prevent serious medical events including blood clots, strokes, and heart failure.[3]
Download your free copy of the report at www.pbmi.com/specialtyreports.
The report is free but requires a free PBMI website account. Once logged on,
add the report to your cart and go through the checkout process.
How Employers Are Combating the Trend?
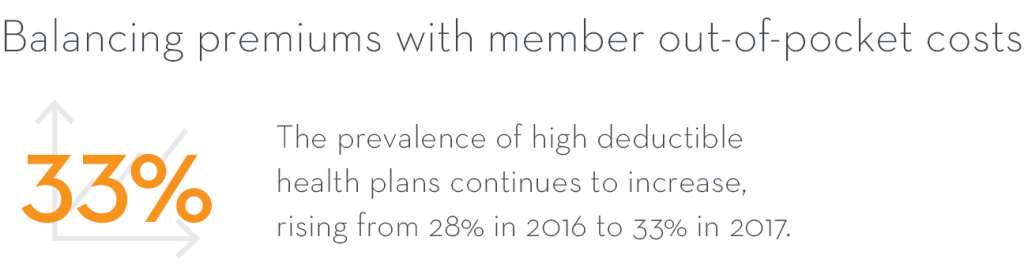
This does not mean employers are standing still. Far from it. Employers are making difficult choices about cost-sharing and plan design. A third of employers have moved to high deductible health plans as a way to encourage members to make better decisions while keeping premiums as affordable as possible.
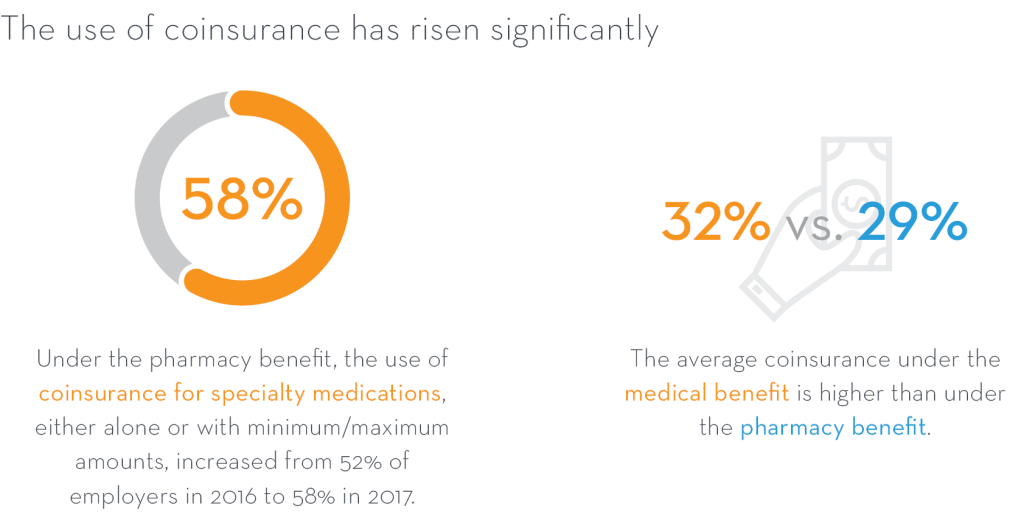
In recognition that only 1-2% of members use specialty drugs, 56% of employers have a separate cost-sharing tier for specialty drugs and 58% use coinsurance for cost-sharing versus flat copayments.
Through the use of clinical utilization management (UM) tools and drug benefit design, employers strive to balance cost management with member access to these, often life-saving drugs, and provide a quality drug benefit for all of their members. Prior authorization is almost universally used and step therapy programs for specialty drugs are in place for 85% of employers. Clinical care management programs and limits on days’ supply are also commonly used.
Specialty Clinical Management Strategies Used in the Pharmacy Benefit
More than half of employers (58%) exclude certain specialty drugs altogether. Formulary exclusions are most common in drug classes with several options such as those used to treat hepatitis C, inflammatory conditions such as rheumatoid arthritis, fertility, and multiple sclerosis. More than 60% of employers agree that formulary exclusions are a good way to manage specialty trend.

Employers don’t go it alone either. They turn to experts – consultants, their PBM, their health plan, and others to help make informed decisions. There is still room to find ways to manage drug spend responsibly including:
- Site of care management, especially under the medical benefit where only 31% of employers use cost-sharing design to encourage the use of lower-cost sites of care
- Specialty drug reporting under the medical benefit – only 48% of employers receive reporting on drug cost

Employers want to provide quality drug benefits. They also have a financial responsibility. Managing specialty drugs well requires constant monitoring and often flexibility to make changes in an ever-evolving market.
For more details, download your free copy of the report at www.pbmi.com/specialtyreports.
The report is free but requires a free PBMI website account. Once logged on, add the report to your cart and go through the checkout process.
_____________________________________________________________________________________________