Carving Out Pharmacy Benefit Solutions: The Changing Landscape of Pharmacy Benefit Management
Posted on November 2, 2023
It is estimated that 6.7 billion prescriptions were dispensed in 2022 [1], while 70% of US adults report taking at least one prescription per day[2]. The pharmacy benefit is the most accessed by patients, and the large majority of prescriptions dispensed are managed by pharmacy benefit managers (PBMs). The PBM industry is notably highly consolidated, with the three largest firms controlling nearly 80% of the market share. Investment dollars from the likes of Fortune 10 companies and notable celebrities are flooding into the industry, with hopes of disrupting a highly profitable industry.
Far too often, the voice of pharmacy benefit buyers is lost in the constant churn of insights on the PBM industry. For over two decades, PSG’s Pharmacy Benefit Manager (PBM) Customer Satisfaction Report has provided unbiased insights into the perspectives of buyers of PBM services, which include health plans, employers, and labor unions. This year’s report revealed several key trends that may point to the beginning of a shift in how plan sponsors holistically procure their benefits.
The Decline in PBM Satisfaction
The 2023 PBM Customer Satisfaction Report surveyed nearly 230 representatives of health plans, employers, labor unions, and other similar organizations, and unveiled an interesting trend. PBM satisfaction has dipped from 8.2 to 7.6 on a customer satisfaction scale ranging from 1 (not at all satisfied) to 10 (extremely satisfied). This marks the lowest point since 2014, and other high-level metrics, like likelihood to recommend and are also declining. The decline in NPS was particularly noteworthy, dropping from 38 to 8 in just two years. Considering payers’ struggles with drug spend and trend and the negative public attention PBMs are receiving, these declines are not surprising.
Carving Out PBM Services: A Compelling Option
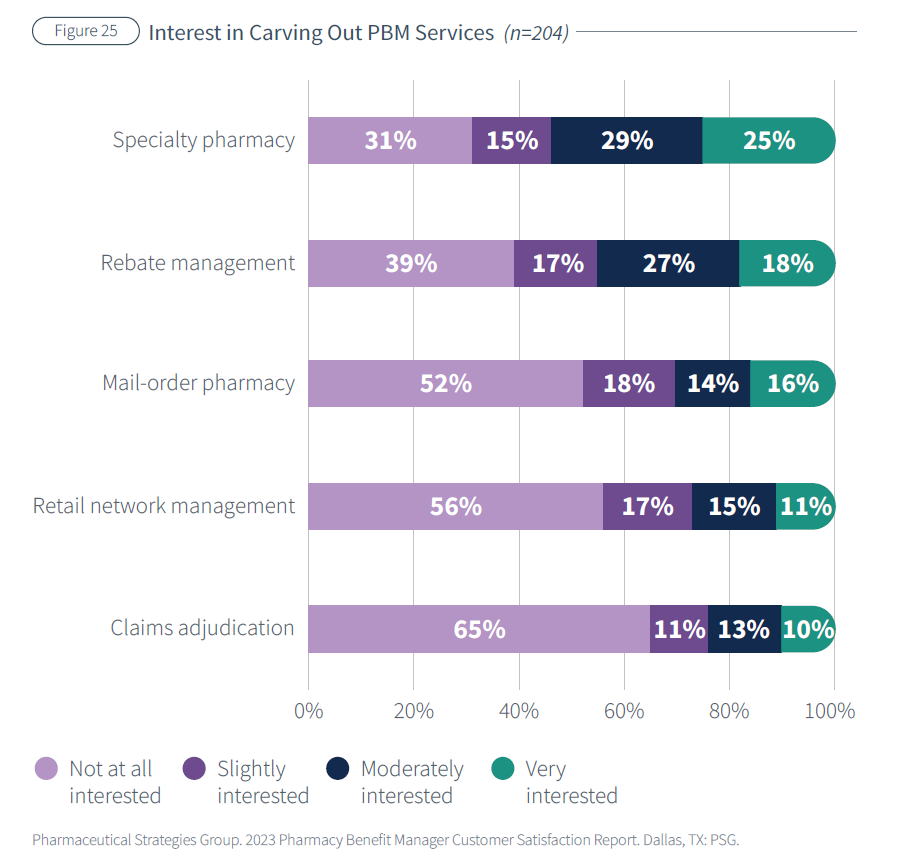
Given the current declines in high-level satisfaction with PBMs, it’s no surprise that stakeholders are exploring alternatives. Our survey confirmed this theory, with results showing substantial interest in carving out certain PBM services and outsourcing them to standalone vendors. Notably, there is a strong inclination to carve out specialty pharmacy services and rebate management, with around 40-50% of respondents expressing moderate to high interest in these carve outs. In contrast, respondents were less interested in carving out services like mail-order pharmacy, retail network management, and claims adjudication. With high interest in carving out elements of the PBM solution and PBM satisfaction at a recent low, what does this mean for health plans, employers, and other stakeholders in the pharmacy benefits space?
Health Plan Perspectives on Carve Outs
The news by one of the largest regional health plans to reimagine the PBM model, using multiple vendors instead of a single vendor for pharmacy benefit management services, could be a preview of a significant industry shift in health plan approaches. Health plans have more complex needs and higher standards expected of their PBMs. Complexities such as custom formularies, serving downstream customers, and regulatory requirements cause them to demand more. In our research, we consistently lower health plan ratings of their PBM on nearly all attributes compared to employer responses, reflective of these higher expectations.
Health plans must be mindful of their approach. The reasons for disintegration vary by plan but often involve a desire for transparency and greater control. However, an unbundled model has risks and challenges. There are obvious considerations, according to PSG’s Michael Kolodij, PharmD, in a recent webinar. These include ensuring a seamless patient experience and the ability to share information and data across vendors. However, there are also less obvious considerations. One example is Medicare compliance, as many plans rely on their PBM to be consultative experts on this topic when setting up the pharmacy benefit. Another key consideration is ensuring financial competitiveness of the plan’s pharmacy offering. The premise of fully disruptive solutions is that enough middlemen are earning margin in today’s model that carving out and shortening the supply chain will result in a more affordable benefit. We affirm at PSG this can be true but recognize it requires sophisticated procurement, implementation, and operational strategy to accomplish that goal.
Employer Perspectives on Carve Outs
Employers, on the other hand, have different considerations. Carving out services may entail adding more administrative support for managing vendor relationships. Employer benefit decision makers are often tasked with managing a portfolio of total rewards including pharmacy, medical, mental health, and financial programs. We observe that employers are often motivated to carve out certain aspects of the pharmacy program to improve the member experience, and the area most frequently carved out is specialty pharmacy. In recent years, vendors focused on specialty management have presented compelling value propositions that some employers have adopted or have strong interest in. Employers should consider the sustainability of these carve out specialty solutions with an eye toward whether the program is leading to better specialty therapy management. For example, alternative funding programs have grown in popularity due to the promise of immediate savings, but many stakeholders question the long-term sustainability and ethical implications of those programs.
Leveraging Industry Insights
In this ever-evolving landscape, staying informed is essential. Leveraging the knowledge and expertise of industry experts is undoubtedly valuable, and research reports can provide an accessible and comprehensive view of the market.
Our annual research report on PBM Customer Satisfaction is available for download below, offering a deeper dive into the findings discussed here and more.
So, what lies ahead for disruptive services in the pharmacy benefits space, and are these efforts sustainable? Only time will reveal the answers. But in the meantime, we encourage you to explore industry data and educate yourself to make informed decisions that will best support your business!
Download the 2023 PBM Customer Satisfaction Report

[1] https://www.iqvia.com/insights/the-iqvia-institute/reports-and-publications/reports/the-use-of-medicines-in-the-us-2023
[2] https://civicscience.com/a-growing-number-of-americans-report-taking-prescription-medications-daily/

