Upcoming 2020 Formulary Changes – PSG Key Insights
Posted on October 29, 2019
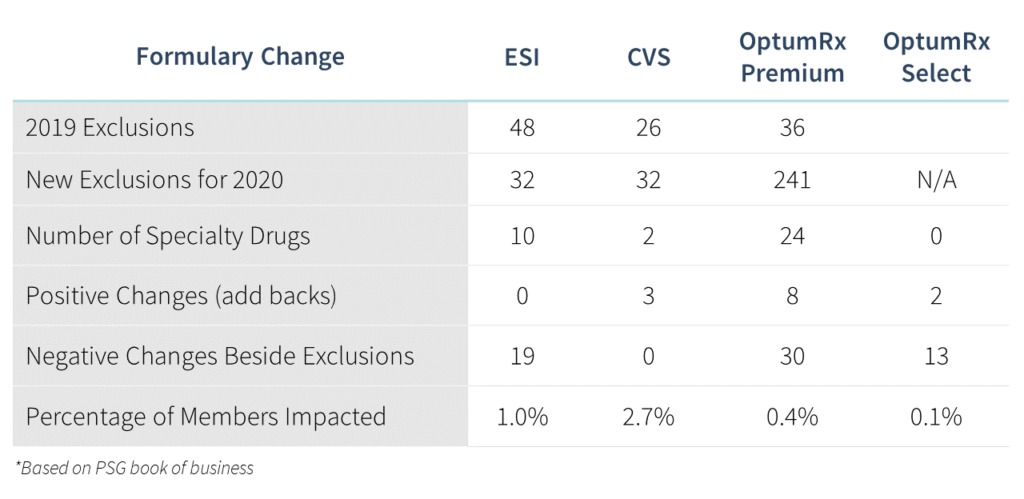
The Big Three Pharmacy Benefit Managers (OptumRx, Express Scripts, CVS Caremark) released updates to their 2020 formulary exclusions, and our analysis shows that member impact from the changes varies considerably among the three. The number of changes for Express Scripts and CVS is limited compared to the 241 exclusions from OptumRx. The large number of OptumRx’s exclusions include the removal of 192 multi-source brands (including Lyrica, Ranexa, Suboxone, Synthroid, Vesicare) and the addition of therapeutic equivalents for the Premium formulary.
The Big Three are continuing to work toward a better understanding of the unique needs of their clients. A few innovative strategies we will see implemented next year include a flex formulary for Express Scripts, a brand-over-generic strategy for CVS, and variations in coverage for biosimilars, hyperinflationary drugs, and continuous glucose monitors.
The findings of an impact analysis across our book of business suggest the changes will impact 1.6% of members and 2.8% of total drug spend. This chart summarizes the changes:
Want to find out how these changes may affect you? Contact PSG today to get the formulary strategy and support you need for an ever-evolving market.
Highlights of the most notable formulary changes are discussed below.
CVS expands brand-over-generic
CVS will implement a Tier 1 approach to deliver lowest net cost. This move will allow coverage of a brand drug on the first tier if the brand is the lowest-net-cost option. The brand will process with a generic copay, and the generic will be excluded from coverage. Adderall XR, Concerta and Advair will be the first three drugs in this new program.
All patients utilizing those medications will be transitioned to the brand-name drugs at the beginning of the year. While members will benefit from the Tier 1 copay, it is unclear if plan designs for all plan sponsors can support generic copays for brand-name drugs. In addition, with the longevity of the program unknown, there is a risk of member disruption if, and when, covering the brands no longer makes financial sense.
Biosimilar strategies offer a mixed bag
OptumRx, as part of their first-mover initiative, will replace Avastin and Herceptin with their respective biosimilars. Express Scripts will prefer Zarxio and Nivestym, the biosimilars for Neupogen, instead of Granix, but will exclude coverage of Fulphila, a biosimilar for Neulasta. CVS has included some biosimilars in preferred positions on their Advanced Control Specialty Formulary, including Nivestym, a biosimilar, instead of Neupogen, while also including both Udenyca, a biosimilar for Neulasta, and brand Neulasta. The uptake of biosimilars in the U.S. market has been slow, but these formulary changes are a start to increase their use. Avastin and Herceptin, drugs that are physician-administered, and Neupogen, to some extent, allows the use of these biosimilars to be overseen by the physicians administering. While we don’t expect any negative clinical impact on members, the use of the biosimilars will be assessed and monitored by the physicians administering the drugs. CVS’ approach of giving equal status to both the biosimilar and brand drug Neulasta will allow coverage for both and utilization of the biosimilar should physicians and members so choose.
What to expect with hyperinflationary drugs and glucose monitors
Hyperinflationary drugs Duexis (ibuprofen + Pepcid) and Vimovo (naproxen + Nexium) continue to be covered on the National Preferred Formulary for Express Scripts but excluded from the National Preferred Flex Formulary. CVS is allowing a path to coverage via medical necessity for drugs such as Glumetza and Fortamet (branded, delayed-release metformin), as well as many dermatology products including Noritate, Alcortin A and Bensal HP. None of these drugs offer any additional clinical value over very low-cost formulary alternatives, especially for drugs like Duexis and Vimovo, when the exact same drugs are available separately and over-the-counter. Clinically, we expect these changes to have little to no impact on members.
FreeStyle Libre, the continuous glucose monitor (CGM) with the lowest upfront price point, is being removed from the CVS Standard Control Formulary and replaced with the high cost CGM, Dexcom G6, as the preferred agent. Similarly, OptumRx Premium Formulary will exclude FreeStyle Libre and move Dexcom G6 to the preferred position, making this formulary strategy completely reliant on rebates to make up for any plan paid differences in costs. Impacted members will be required to obtain a new system based on the preferred formulary product, which may include a handheld reader, receiver or application on their smart device, as well as compatible sensors and applicators. The continuous glucose monitors are comparable in the accuracy of glucose readings. However, members will need to become familiar with how to operate the new device. Dexcom G6 can send readings directly to a smart device, while the Freestyle Libre will require scanning of the sensor to obtain the reading. Due to differences in price, members with a cost-share or deductible may notice a higher out-of-pocket amount for the Dexcom G6.
PSG has developed a review of each of the Big Three PBMs and is providing insights into the changes plan sponsors can expect in 2020. If you would like more information on another PBM not represented here, please contact us at [email protected].

