Trends in Specialty Drug Benefit Design: Member Engagement
Posted on June 8, 2022
Employers need to strike the right balance when making decisions about specialty drug benefits. So much of the conversation around specialty drugs, understandably, tend to focus on managing costs and affordability of benefits. But it’s important to also keep in mind the return on investment (ROI) of these benefits for your organization.
Understanding how your specialty drug benefit design enhances member engagement can help you create a better benefits plan and create more significant long-term value for your organization and members.
Let’s look at why member engagement must be central to your specialty drug benefit plan design and overall strategy for administering these benefits.
Back to basics: Why offer specialty drug benefits?
It’s worth re-examining the strategic imperative for offering specialty drug benefits. Of course, your company cares about your people, and you want to help them get the medications they and their families need. But it’s critical to reassess your True North for why specialty drugs are part of your benefits package and what you’re hoping to accomplish by offering these benefits.
The three biggest reasons to offer specialty drug benefits include:
- Invest in employee wellbeing
This reason is perhaps most crucial. You need to keep employees healthy and invest in their overall wellness. Providing access to clinically appropriate specialty drugs is critical to achieving this goal. Healthy employees who feel supported by their employer are more likely to keep working for your organization.
- Reduce absenteeism and improve productivity
On a fundamental level, people need to be healthy to show up for work and achieve peak productivity during work hours. Getting access to the correct prescription medication can make a big difference.
- Recruit and retain key talent
Your best-performing employees will be more likely to jump ship for another job if they can’t get the specialty drug coverage they need or repeatedly face frustrations, delays, and hassles in getting their prescriptions.
For these reasons and more, specialty drugs are top-of-mind for plan sponsors.
Why specialty drugs cost so much—and why they’re so important
Specialty drugs can be hard to define. There is no single clear, universally accepted legal definition. But in general, we define specialty drugs as:
- Treats a chronic, complex or rare condition
- Requires specialized handling or storage
- Requires specialized patient care coordination
- High cost
- Available through a limited distribution network
The cost factor of specialty drugs tends to get a lot of attention in public discussion around prescription drugs. After all, specialty drug prescriptions represent a large percentage (50% or more) of employers’ overall drug spend. However, these costs also help provide significant value to patients and organizations. Specialty drugs represent scientific advancements that significantly impact members’ lives by providing specialized treatments or powerful cures to challenging medical conditions.
Recent scientific advances in specialty drug development have enabled millions of patients with serious health conditions to live decades longer than previous generations might have imagined. Specialty drugs not only save lives, they improve the quality of life. For many patients, the use of specialty drugs are not as one-time cures but as longer-term therapeutics for chronic health conditions.
Bottom line: specialty drugs might be costly, but those costs deliver life-changing, life-extending value to patients. There are good reasons that justify investing in specialty drugs despite their high costs.
Navigating complexity: Dual payment methodology
Another reason why specialty drugs tend to be more costly and complex to administer is their dual payment methodology. This means some specialty drugs are paid under the plan’s pharmacy benefit, medical benefit, or both. The exact payment methodology depends on the drug, and the organization’s benefit plan design, route of administration, and site of care.
Another factor that adds to the complexity is dispensing specialty drugs through various channels, such as pharmacies (mail-order, retail, or specialty pharmacies), physician offices, outpatient clinics, infusion centers, or home infusion. Not all of these channels offer the same level of tracking, care coordination, and reporting on drug utilization and costs.
As part of your specialty drug benefit design, try to account for these complexities and look for opportunities to control costs while ensuring access for patients.
Benefit design: Consider all factors
When designing a specialty drug benefit, it’s essential to include a few key considerations:
- Financial considerations
These include budget, past and projected trends, benefit structure, and cost-sharing.
- Clinical considerations
Which specialty drugs will you cover with your plan, which clinical utilization management (UM) programs to use, and how can you make sure you’re your members can access the most appropriate channels and sites of care?
- Sociodemographic considerations
What is your corporate culture, and how does it affect your approach to benefits? What are your employees’ ages, education levels, health status, and other demographic aspects of your workforce? Employee wages will also affect your plan design; higher-paid employees will be better able to afford cost-sharing.
Keeping these considerations in mind will help you design a more effective specialty drug benefit plan that suits the unique needs of your workforce and your organization.
Track Metrics and Outcomes
Many organizations focus on tracking their drug spending, which is important but not sufficient on its own. Achieving the best ROI from your specialty drug benefit plan while maximizing the benefits to your employees’ health and wellness requires comprehensive specialty drug management. This includes accurate tracking of metrics and outcomes.
According to our recent “Trends in Specialty Drug Benefit Design Report,” 85% of benefits leaders are currently tracking total healthcare costs for members using specialty medications, and 82% are tracking specialty drug net costs after subtracting rebates and discounts.
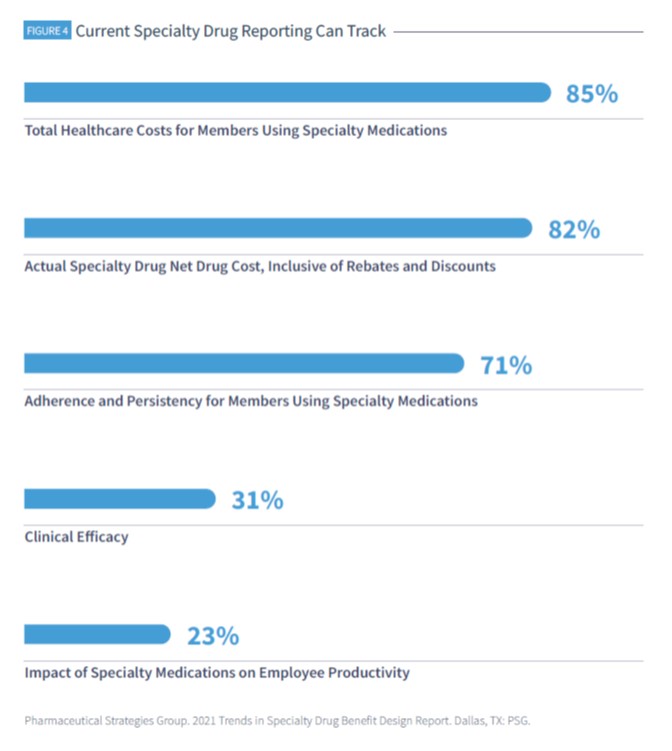
However, clinical outcomes are getting tracked less often. Our survey found:
- Only 71% of benefits leaders are tracking their members’ medication adherence and persistency
- 31% are tracking the clinical efficacy of their plan’s covered specialty drugs
- 23% are tracking the impact of specialty medications on employee productivity
These other metrics are important to your members’ wellness, and they should be part of your plan’s overall tracking and assessment. Remember the list of biggest reasons why employers offer specialty drug benefits? Improving productivity is one of the strategic imperatives for offering specialty drug benefits, so why not track it?
Understanding the upside and ROI of specialty drugs and their costs can help your organization design a more strategically focused, more employee-centric, and more effective benefit plan.

